The Real Reason Republicans Want to Pull the Plug on Obamacare
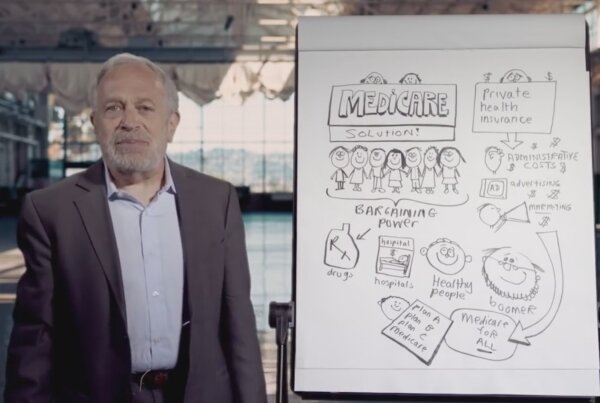
The real reason Republicans want to pull the plug on Obamacare, according to Robert Reich.



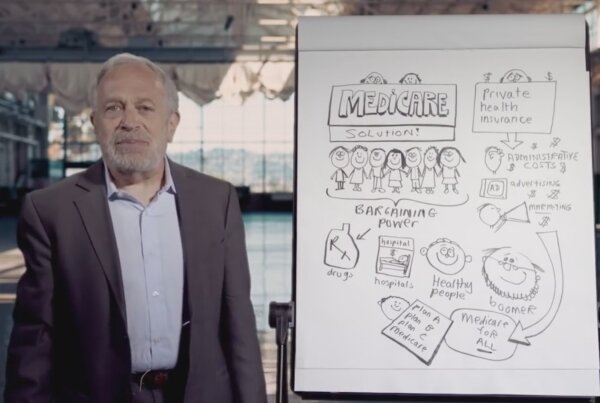






The real reason Republicans want to pull the plug on Obamacare, according to Robert Reich.